
Researchers at the University of Mississippi Medical Center are using post-mortem brain tissue to study biological changes in major depressive disorder. Working on the project are (left to right) Dr. Jose Miguel-Hidalgo, Dr. Grazyna Rajkowska and Dr. Craig Stockmeier.
JACKSON, Miss. – Depression is more than just sadness. Sufferers may lose interest in favorite activities or lose motivation to complete routine tasks. They may also lose some brain cells, say University of Mississippi Medical Center neuroscientists.
According to a study in the March issue of Neuroscience, people with major depressive disorder, or MDD, may have fewer glial cells called astrocytes in some parts of the brain’s hippocampus.
Glia, from the Greek for “glue,” were long thought to be just structural cells keeping everything stuck together. But Dr. Grazyna Rajkowska, professor of psychiatry and human behavior, was one of the first scientists to show a connection between fewer glia and depression.
“People thought depression had to do with neurons. No one thought about glia,” Rajkowska said. “The decrease in glial density is much more dramatic than the changes in neurons.”
“She’s the grandmother of glia and depression,” joked Dr. Craig Stockmeier, professor of psychiatry and human behavior.
But Stockmeier is also serious about studying the brain.
“Seeing the struggles and tragedy of mental illness in acquaintances and extended family is a deep personal motivation for my work,” he said.
For more than 15 years, Rajkowska, Stockmeier and Dr. Jose Miguel-Hidalgo, associate professor of psychiatry and human behavior, together have studied the brain’s cellular and biochemical changes in mental illness, including this recent study.
The team collected brain tissue from 17 recently deceased people with a history of MDD symptoms, then matched each sample with a non-MDD control by age and gender.
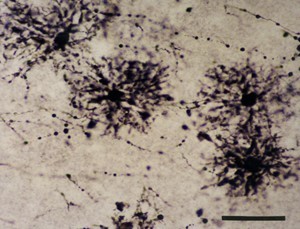
Microscope image of astrocytes (dark) in the hippocampus.
The tissue was cut into sections 40 microns thick, thinner than most human hairs. Then the scientists identified astrocytes by treating the cells to look for glial fibrillary acidic protein, or GFAP, a protein they contain.
Astrocytes are glial cells that transport and recycle chemicals in the brain. Stockmeier compares their role to delivery and garbage trucks: if you take away the trucks or they aren’t working properly, then materials build up. Some of those materials are neurotransmitters such as glutamate and GABA, which send signals between cells.
Depression occurs when those signals are lost or hindered, Miguel-Hidalgo said.
“There are studies in animal models showing that when you kill glial cells, this causes depression-like symptoms,” Rajkowska said.
They found that MDD patients who were not taking medication had 26 percent fewer astrocytes in parts of the hippocampus than healthy subjects or those who were taking antidepressants.
The hippocampus is the brain area crucial to memory, learning and navigation. Learning and memory problems can occur due to chronic stress, which can also contribute to the development of depression, Stockmeier said.
However, they cannot determine if antidepressant use restored the astrocytes or prevented them from being lost in the first place. In either case, Stockmeier and Rajkowska think that treating depression earlier may lessen astrocyte pathology and protect neurons.
They also found that older subjects with depression had a greater area of GFAP immunoreactivity in part of the hippocampus. This could mean that cells get bigger or are more densely packed, which could limit the number of connections between cells and contribute to MDD, Stockmeier said.
In the paper, the researchers suggest that the link between astrocyte loss and MDD involves stress-related corticosteroids. When this hormone builds up, it changes the communication and connectivity between cells, which may contribute to depression, Miguel-Hidalgo said.
“But can you quantify how biochemical changes in the brain relate to different behaviors?” Miguel-Hidalgo asked. For example, some depression types are associated with elevated corticosteroids and others with decreased levels, he said.
This is one of many unanswered questions regarding depression. Another is the causes of depression: they may be a combination of genetic and environmental factors.
“The brain can be affected by experiences and other systems in the body,” such as early-life events, drug and alcohol abuse or the microbiome, Stockmeier said.
The symptoms of depression are also quite variable.
Dr. Scott Rodgers
“While most patients suffer from insomnia, some patients actually experience the opposite problem, hypersomnia,” said Dr. Scott Rodgers, professor and chair of psychiatry and human behavior. “The same is true for appetite. Most patients lose their appetite, but a significant number of people experience an increase in appetite.”
Furthermore, depression symptoms can be shared with other illnesses, Stockmeier said.
“There has been a call for more consistent diagnostic measures of depression, with a greater focus on common biological markers” he said.
A patient’s symptoms and history determine which treatments a clinician may consider; the more severe the symptoms, the more likely a medication will be prescribed, Rodgers said.
“There has been some promising work focusing on glutamate (as a biochemical target for new antidepressant medications),” he said. “Whether a new FDA-approved antidepressant class emerges as a result remains to be seen.”
The UMMC team’s study has a couple of limitations. Seventeen individuals is a small sample and only seven of those were using antidepressants near the time of their deaths. Further, cross-sectional studies like this provide only a snapshot in time, not the entire progression of a patient’s illness. You have less control over study conditions, Rajkowska says.
However, the study’s findings do help understand the brain pathology associated with depression.
“The brain is the most complex organ of the human body,” Rajkowska said. “With each research project, we are getting a bit closer to understanding how the brain is built and how it functions.”
Likewise, Miguel-Hidalgo sees researching the brain as a fascinating project.
“This search is an almost never-ending source of science and wonder,” he said.
This research was funded by a grant from the National Institutes of Health through its Center of Biomedical Research Excellence program.